
VIU Students Helping Most Vulnerable Victims of Opioid Crisis
October 17, 2018 - 9:45am
By Aly Winks
People who experience childhood trauma often describe the event as life-changing, and rarely for the better. Research suggests that early intervention after such events can make all the difference in a young person’s life. That’s where VIU Child and Youth Care students and faculty hope to make an impact.
British Columbia is currently in the middle of a medical health crisis that is leaving untold numbers of traumatized children in its wake. Every day, the opioid crisis takes the lives of about four individuals in the province, according to the BC Coroner’s Service. Its collateral damage includes children who have lost parents, grandparents, aunts, uncles and other loved ones to overdose deaths. Others are affected in less direct ways, such as through the media or having other adults or friends in their lives who are users.

Community in Crisis
Simply keeping people alive after fentanyl and carfentanil poisonings has frontline workers burnt out – emotionally and physically exhausted from what they see and do every day. Aside from these obvious victims of the opioid crisis are their family members and friends.
It was in this context that Child and Youth Care students at VIU started asking what was happening to the children who are involved in the crisis – and discovered a gap in support.
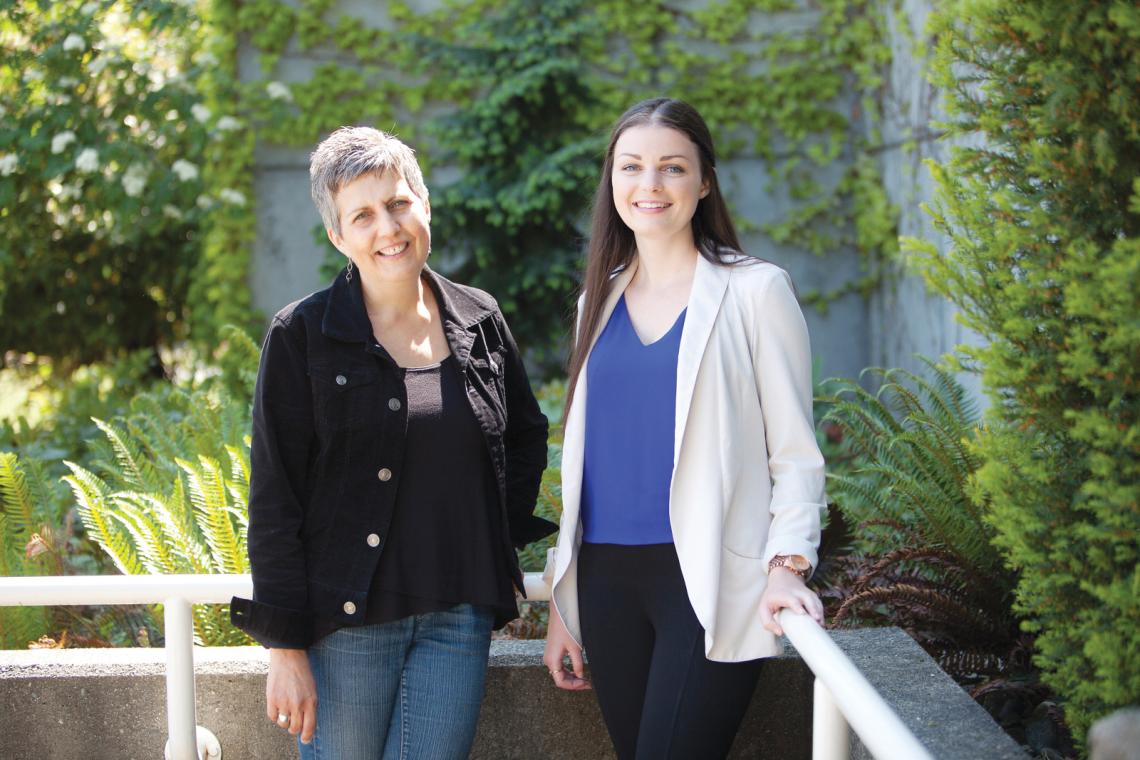
Emma Gillis is one of those students. She began her degree with an interest in addiction, but did not know where her education might lead her. When the opportunity for her practicum came up, this topic and its unseen victims drew her in.
“We just kept asking ourselves, ‘What is happening to the children?’” the fourth-year student says. “Statistics show that most poisonings happen in homes or buildings, and wherever there are homes, oftentimes there are children. There was a gap for the most vulnerable people in our population. To compound the tragedy, we know that early treatment in dealing with trauma can make all the difference in a young person’s life.”
This led Gillis to develop, for her practicum through VIU’s Centre for Community Outreach and Care (CCOC), a program that aims to help children touched by the opioid crisis.
However, nothing is ever as straightforward as it seems and Gillis, along with her mentor, Child and Youth Care Professor Teri Derksen, quickly realized simply getting in touch with their target audience was a considerable challenge.
“We started reaching out to various community organizations as we thought we may be able to build a coalition to get the required care to these children. The groups we spoke to were receptive and our current coalition includes Island Health, NARSF Programs Ltd. (NARSF), and the BC Ministry of Children and Family Development,” Gillis says.

Breaking Down Barriers
Gillis and her partners discovered the biggest obstacle to helping this vulnerable group of children is the stigma that surrounds those who engage in substance use and their loved ones.
“Our community partners kept talking about how hard it is to get people who are facing these challenges to come in and discuss their problems,” says Derksen. “The shame people experience stops them from getting help. So, the people who see their children suffering from the epidemic may feel so guilty they almost can’t do anything.”
Recognizing this, Gillis, Derksen and their team decided the best way forward was to develop some communication with the professionals who work with these groups. From there, they would be able to determine how to eliminate barriers to accessing services and programs.
Long-term work with community groups takes funds, and time was running out on Gillis’s practicum.
“It started to become a question of what was going to happen when Emma left,” says Derksen.
Next Steps
Gillis did not want to leave with the work unfinished either. In the midst of developing the programming, they began, with help from their community partners, a hunt for funds.
“We submitted a proposal to the Canadian Institute for Substance Use Research, and we were amazed to find out we were successful for the full amount we requested,” Derksen says. “I think it was a recognition of the importance of the work.”
It was enough to extend Gillis’s position beyond the end of last school year, and enabled them to begin hosting a series of community dialogues at the end of April 2018.
“After we finish talking to community groups, we hope we can gain some traction with people who may want to share their stories. Our plan is to host community dialogues throughout the fall and winter,” Gillis says. “The most direct way to break down the stigma is to humanize the issue. The more people relate to each other, see themselves in each other, the more likely they will be able to accept these challenges for what they truly are.”
So what, exactly, are these challenges from Gillis’s perspective?
“There are no stereotypical drug users. Addiction does not discriminate. We need an integrated approach that reflects the needs of the people who are living these experiences every day,” Gillis says. “The more we humanize the people behind the crisis the better all aspects of treating it can be. This includes prevention. If we have programming for these kids that helps them work through growing up around substance use, we can decrease the risk of future substance use and addiction — we are can make a real difference.”
Province Launches #StopOverdose Campaign
There is a public health emergency in BC. People are overdosing on illegal substances in high numbers. Drugs like heroin, fake oxys and other illegal opioids can contain toxic fentanyl or carfentanil. Other illegal drugs may be contaminated, too.
The Ministry of Mental Health and Addictions has launched a Stop Overdose BC campaign to challenge people’s perceptions about people who use drugs and call on all British Columbians to get involved, get informed and get help.
Visit StopOverdoseBC.ca for life-saving information, and use #StopOverdose to join the conversation online.
How You Can Help *:
1 Start courageous conversations with loved ones
2 Words matter, learn how positive language makes a difference
3 Learn how to recognize and respond to an overdose
4 Make time to thank those working on the front lines of the crisis
5 Get involved – add your voice to the #StopOverdose conversation
6 Call 8-1-1 for non-emergency help and advice, 24/7
*from StopOverdoseBC.ca
*This article originally appeared in the Fall 2018 edition of VIU Magazine. Check out more stories on the VIU Magazine webpage.
Tags: Child and Youth Care | Research | VIU Magazine






